Billy Joel Brings Awareness to Normal Pressure Hydrocephalus
Renowned musician Billy Joel recently disclosed his battle with a rare neurological disorder called normal pressure hydrocephalus (NPH). This condition involves an unusual accumulation of cerebrospinal fluid within the brain’s ventricles, which can disrupt normal brain function. Unlike other types of hydrocephalus, NPH develops gradually and often presents symptoms that resemble other neurodegenerative diseases, complicating timely diagnosis. Joel’s openness has sparked increased public interest and medical discussion about this frequently overlooked illness.
The hallmark symptoms of NPH typically include:
- Walking difficulties: a slow, shuffling gait or trouble initiating steps
- Mental decline: memory lapses, confusion, and reduced concentration
- Bladder control issues: frequent urination or incontinence
To better understand NPH, here is a comparison with other neurological disorders it is often mistaken for:
| Disorder | Primary Symptoms | Disease Course |
|---|---|---|
| Normal Pressure Hydrocephalus | Gait problems, cognitive decline, urinary incontinence | Gradual onset, potentially reversible |
| Alzheimer’s Disease | Memory loss, disorientation, mood swings | Progressive and irreversible |
| Parkinson’s Disease | Tremors, muscle stiffness, slowed movement | Chronic and worsening over time |
Normal Pressure Hydrocephalus: Overview, Symptoms, and Origins
Normal Pressure Hydrocephalus (NPH) is a neurological disorder characterized by an abnormal increase of cerebrospinal fluid in the brain’s ventricles, yet with normal intracranial pressure readings. This subtle fluid buildup can cause symptoms that overlap with other brain diseases, making it a diagnostic challenge. The classic symptom triad includes:
- Walking abnormalities: patients often experience a broad-based, slow, or shuffling gait.
- Cognitive difficulties: issues with memory, attention, and problem-solving.
- Urinary problems: urgency or loss of bladder control.
NPH is categorized into two types: idiopathic, where the cause remains unknown, and secondary, which arises due to factors such as head injuries, strokes, infections, or brain surgeries. Although it predominantly affects older adults, recent studies estimate that up to 5% of individuals over 65 may have undiagnosed NPH, highlighting the need for increased vigilance. Early recognition and intervention can dramatically improve patient outcomes.
| NPH Type | Typical Causes | Dominant Symptom |
|---|---|---|
| Idiopathic | Unknown origin | Gait disturbance |
| Secondary | Stroke, trauma, infection | Cognitive decline |
Why Early Diagnosis of NPH Is Vital
Detecting normal pressure hydrocephalus at an early stage is crucial to prevent permanent neurological damage and to maximize treatment success. Because NPH symptoms often resemble those of Alzheimer’s or Parkinson’s diseases, it is frequently misdiagnosed or overlooked. Identifying the subtle combination of gait impairment, urinary incontinence, and mild cognitive issues allows healthcare providers to initiate appropriate interventions sooner.
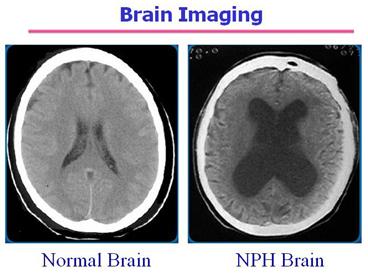
Delayed or incorrect diagnosis can lead to worsening symptoms and reduced chances of recovery. Comprehensive neurological assessments, including MRI or CT scans, are essential tools to distinguish NPH from other disorders. According to recent clinical data, patients who receive treatment within six months of symptom onset have a 70% chance of significant improvement.
- Enhanced treatment outcomes: Early diagnosis increases the likelihood of successful surgical intervention.
- Potential symptom reversal: Walking ability and cognitive functions can improve markedly.
- Lower healthcare burden: Avoids unnecessary treatments and hospitalizations.
- Prevention of brain damage: Stops progression of ventricular enlargement and tissue injury.
| Factor | Early Diagnosis | Late Diagnosis |
|---|---|---|
| Symptom Improvement | High likelihood | Low likelihood |
| Treatment Effectiveness | More effective | Limited options |
| Quality of Life | Significantly improved | Declines over time |
| Risk of Complications | Reduced | Increased |
Managing NPH: Treatment and Lifestyle Strategies
Addressing normal pressure hydrocephalus involves a combination of surgical and supportive care approaches. The primary treatment is the surgical insertion of a ventriculoperitoneal (VP) shunt, which diverts excess cerebrospinal fluid from the brain’s ventricles to the abdominal cavity, thereby relieving pressure. This intervention often results in notable improvements in mobility, bladder control, and cognitive abilities. However, patient outcomes can vary, and ongoing monitoring is essential to detect potential complications such as shunt malfunction or infection.
Complementary therapies play a vital role in enhancing daily functioning and quality of life. Physical therapy focuses on improving balance and gait, while occupational therapy supports patients in maintaining independence with everyday tasks. Additionally, cognitive training exercises and a nutritious diet may contribute to brain health. Caregivers should stay informed about symptom changes and ensure regular medical follow-ups.
- Routine neurological check-ups to monitor disease progression
- Periodic brain imaging to evaluate ventricular size and shunt function
- Rehabilitative therapies to optimize mobility and self-care skills
- Support networks offering emotional and educational resources
| Treatment | Goal | Expected Benefit |
|---|---|---|
| Ventriculoperitoneal Shunt | Drain excess cerebrospinal fluid | Improved gait and cognition |
| Physical Therapy | Enhance strength and balance | Reduced fall risk and better mobility |
| Occupational Therapy | Support daily living activities | Greater independence |
| Ongoing Monitoring | Detect complications early | Timely treatment adjustments |
Final Thoughts on NPH Awareness and Treatment
Billy Joel’s public disclosure of his normal pressure hydrocephalus diagnosis has helped shine a spotlight on this rare but treatable brain disorder. Recognizing the early signs and seeking prompt medical evaluation are essential steps toward effective management. While NPH is often confused with other neurological diseases, it stands apart due to its potential reversibility with timely intervention. Joel’s story underscores the powerful impact that public figures can have in raising awareness, fostering understanding, and encouraging those affected to pursue diagnosis and care.