Addressing the Persistent Opioid Crisis Among U.S. Veterans
National Trends Show Decline in Opioid Deaths, Yet Veterans Face Rising Risks
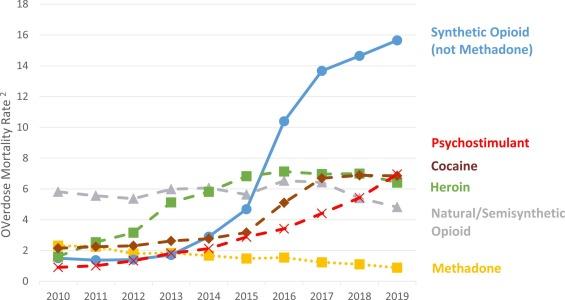
While the United States has witnessed a notable reduction in opioid-related fatalities over recent years, this encouraging trend does not extend uniformly to all populations. Veterans, in particular, continue to suffer from disproportionately elevated rates of opioid overdose and addiction. Despite advances in public health initiatives and treatment modalities, the veteran community grapples with distinct challenges—such as chronic pain management, mental health disorders, and social disconnection—that complicate recovery efforts and prevention strategies.
Several critical factors contribute to this ongoing crisis among veterans:
- Limited availability of addiction treatment programs tailored specifically to veterans’ needs
- Fragmented integration of mental health services with pain management approaches
- Persistent stigma around substance use within military and veteran circles
- High prevalence of PTSD and traumatic brain injuries that intensify opioid dependency
| Group | Annual Opioid Death Rate (per 100,000) | Change Over Last 5 Years |
|---|---|---|
| General Population | 12.4 | -18% |
| Veterans | 21.7 | +3% |
Challenges Hindering Effective Addiction Treatment for Veterans
Despite nationwide improvements in opioid overdose prevention, veterans encounter unique barriers that limit their access to effective addiction care. Many specialized programs that address military-specific trauma and cultural nuances remain scarce. Additionally, stigma within the veteran community often discourages individuals from seeking help, fostering isolation and untreated substance use disorders. The frequent co-occurrence of mental health conditions such as PTSD further complicates treatment, requiring integrated approaches that are not always available.
Structural limitations within the Veterans Health Administration (VHA) exacerbate these issues. Veterans living in rural or underserved areas face long wait times, transportation difficulties, and bureaucratic obstacles that delay or prevent treatment. Below is an overview of the primary barriers and potential solutions:
- Scarcity of specialized care: Few programs combine addiction treatment with trauma-informed approaches.
- Stigma and mistrust: Concerns about judgment or career repercussions reduce treatment-seeking behavior.
- Geographic and logistical hurdles: Distance, transportation, and appointment availability limit access.
- Fragmented healthcare services: Lack of coordination between mental health, physical health, and addiction care providers.
| Barrier | Effect on Veterans | Recommended Intervention |
|---|---|---|
| Limited Specialized Programs | Insufficient trauma-sensitive addiction care | Establish integrated veteran-focused treatment centers |
| Stigma | Reluctance to seek help | Expand confidential peer support and counseling services |
| Geographical Barriers | Lower treatment adherence in remote areas | Increase telehealth services and mobile outreach units |
| Service Fragmentation | Disjointed care reduces recovery outcomes | Implement coordinated care models linking mental health and addiction services |
Enhancing Mental Health Support to Reduce Veteran Overdose Rates
Robust mental health care is a cornerstone in preventing opioid overdoses among veterans. Conditions such as PTSD, depression, and anxiety frequently co-exist with substance use disorders, making integrated behavioral health services essential. Veterans who participate in consistent counseling, peer-led support groups, and medication-assisted treatment (MAT) demonstrate significantly improved outcomes, including reduced opioid misuse and overdose incidents.
Effective mental health strategies for veterans include:
- Early and routine screening for mental health disorders
- Customized treatment plans reflecting veterans’ unique experiences
- Collaboration between VA healthcare providers and community mental health organizations
- Increased investment in veteran-specific substance use disorder programs
- Public education campaigns aimed at reducing stigma around seeking mental health care
| Mental Health Service | Contribution to Overdose Prevention | Annual Veteran Participation |
|---|---|---|
| Peer Support Networks | Fosters community and reduces isolation | Over 50,000 veterans |
| Medication-Assisted Treatment (MAT) | Mitigates opioid cravings and supports recovery | Available in 70% of VA facilities |
| Cognitive Behavioral Therapy (CBT) | Addresses trauma-related triggers for substance use | Widely offered across mental health clinics |
Policy Reforms Essential to Mitigate Veteran Opioid Vulnerabilities
To effectively combat opioid addiction within the veteran population, policy reforms must be specifically designed to address their distinct needs. Current public health policies often fail to consider the complex interaction of physical injuries, mental health challenges, and military cultural factors that influence substance use. Mandatory comprehensive screening for opioid risk at the point of military discharge is critical for early intervention. Additionally, broadening access to alternative pain management options—such as acupuncture, physical therapy, and cognitive behavioral therapy—can reduce dependence on opioid medications.
Priority policy actions should include:
- Mandatory opioid education programs tailored for veterans and healthcare providers serving them.
- Increased funding and support for partnerships between VA and community organizations to expand treatment access.
- Enhanced prescription monitoring systems to identify and address potential misuse promptly.
| Policy Focus | Current Practice | Recommended Improvement |
|---|---|---|
| Discharge Screening | Voluntary | Mandatory for all veterans |
| Pain Management | Primarily opioid-based | Incorporate alternative therapies |
| Provider Training | General opioid guidelines | Veteran-specific education modules |
Final Thoughts
Although the overall opioid epidemic in the U.S. shows signs of improvement, the persistent increase in opioid-related deaths among veterans reveals a significant shortfall in current public health strategies. To close this gap, it is imperative to develop and implement targeted interventions that address the multifaceted challenges unique to veterans. Without dedicated resources and focused policy reforms, the progress achieved in the general population risks leaving veterans behind in the fight against opioid addiction.